α1-antitrypsin is the most abundant circulating proteinase inhibitor.
Severe deficiency typically results from homozygous inheritance of the Z
allele (Glu342Lys). We showed over 30 years ago that the Z allele caused
α1-antitrypsin to undergo a conformational transition to form chains of
ordered polymers that are retained as inclusions within hepatocytes in
association with liver disease and cirrhosis. We subsequently showed
that many mutations caused α1-antitrypsin to polymerise and that there
was a genotype-phenotype relationship between the severity of the
mutation and the severity of both the plasma deficiency of α1-
antitrypsin and liver disease, that we can explain by the rate of polymer
formation. The same process of polymerisation occurs in mutants of
other serine proteinase inhibitors (serpins), most notably neuroserpin in
association with neuronal inclusions that underlie dementia and
epilepsy. The challenge has been to define the structure of the
pathological polymer that forms in vivo. Three models have been
proposed with our current data supporting the C-sheet model for
polymers of Z α1-antitrypsin. The results allow the rational design of
novel small molecules that can block polymer formation and so
ameliorate disease, whether it be the liver disease secondary to
mutations in α1-antitrypsin or dementia secondary to mutants of
neuroserpin. Different mutations may require different small molecules.
The proof-principle of this approach is our development of orally
bioavailable small molecules with GSK, and now BioMarin, that bind
preferentially to Z α1-antitrypsin, block polymerisation and reverse liver
disease in transgenic mice. These molecules are now in clinical trials.
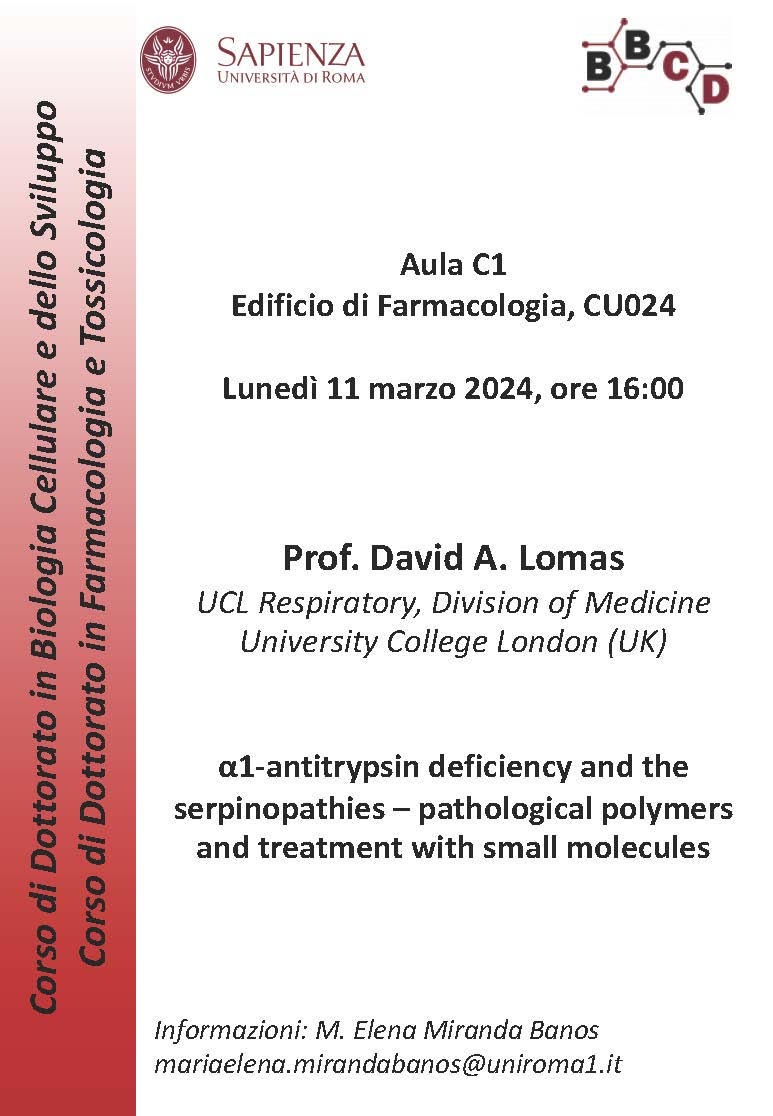
11/03/2024 h 16:00 Room C1 Pharmacology Building CU024
Prof. David A. Lomas
UCL Respiratory, Division of Medicine
University College London (UK)